Action Mental Health (AMH) has teamed up with Dr Jonny Bloomfield for a free all-day NetWalking event at Stormont Estate on Friday 27 June 2025. With a target of 500k steps this charity NetWalk will raise funds for vital mental health services in Northern Ireland, while helping raise awareness and well-being.
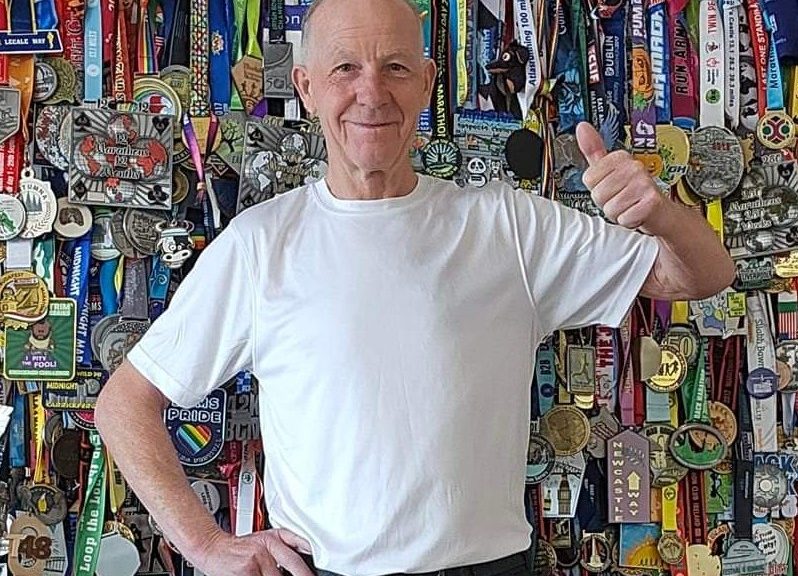
Beginning his career as a fitness coach at Ulster Rugby before becoming a physiologist at the Sports Institute of Northern Ireland, Jonny is well knownas a health and performance coach specialising in stress, sleep, exercise & nutrition. He has 20 years’ experience working in areas of high performance, across different industries and a background in sports science and exercise physiology.
So what exactly is NetWalking? Simply, it is networking while you walk, with this event targeted at anyone who fancies an informal stroll and the opportunity to make new acquaintances while raising funds for mental health. Ticking two of the ‘Take 5’ elements for mental health and well-being; connecting with others and exercising in a green space, NetWalking is widely recognised for its many feel good restorative properties and sense of community.
The concept which originated from ditching the office in favour of talking while walking, has proved very popular as it combines shared experience and the ability to have a conversation without distraction. In the world of business development, NetWalking has quite literally gained a foothold, bringing business people together away from the traditional confines of whiteboards, boardrooms and online meetings, so often associated with traditional networking.
Jonny said, “I’m delighted to be involved with this free NetWalking charity event which will help raise money for mental health services in Northern Ireland. Our usual last Friday of the month netwalk started post-Covid with a regular 10am event from Stormont Estate’s yellow ‘chatty benches’. It is really popular with new people joining every month. We take the route through the woods and then up the hill in front of Stormont, with each person usually clocking up 5000 steps – approximately 3-4 miles. It is an informal event where people are encouraged to partner up.”
“Adding, the AMH charity NetWalk on Friday 27 June 2025 will start at the yellow chatty benches just inside the main gates. This special event offers up the opportunity to be involved in one to five netwalks with starting times of 8am, 10am, 12 noon, 2pm and 4pm. We have a sign-up target of 100 people to collectively achieve 500k steps so please share this event with your family, friends and networks.”
Testimonials from the Last Friday Netwalk at Stormont –
“The Netwalking group has become my benchmark for the month, a space I always look
forward to. It’s welcoming, uplifting, and Jonny sets such a warm, inclusive tone that
meaningful conversation just flows. It is connection, community, and a breath of fresh air all
in one!” – Regular Netwalker, Amanda Barr, Breakup & Divorce Coach
“So glad I joined the Netwalking group for my first dander round Stormont Estate Friday
30th May. Such a welcoming and friendly bunch. Got to have some interesting chats and
meet like-minded people.” – 1 st Timer May 2025, Benny McClure, E M Gray & Co
“Netwalking has been amazing for me. I would usually avoid traditional networking as it can
feel stuffy and forced. This is the exact opposite. Casual and friendly with everyone genuinely
nice and wanting to support each other.” – Regular Netwalker, Matt Greer, Navigate IFA
AMH Fundraising and Engagement Officer, Iain McCarthy said, “As walking and talking helps generate conversation organically, this method of exercise and chatting is a catalyst for creativity, as the rhythm of walking helps with idea formation. Additionally, this informal meeting method helps build connections on a level playing field, making it an enjoyable but dynamic experience. It’s well-being that goes beyond the confines of walls. This event is for everyone from all walks of life and for most fitness levels.”
To get involved please sign up as an individual or group at [email protected]
To donate online please visit: https://www.justgiving.com/page/netwalk-stormont